Everyone wants to know about the effectiveness of medication before they take it.
Similarly, one of the first questions my patients always ask me is how effective their physical therapy treatment will be and how soon they’ll get better.
Answering that question gets complicated because although the treatments we prescribe work for most people, it’s hard to give exact stats on ‘how’ well the treatment will work for a specific patient.
In this article, I’ll try to answer the question of how effective physical therapy is by doing a deep dive into the research papers and treatment protocols available on three of the most common injuries we see in the clinics.
Hopefully, by the end of this article, you’ll understand how each component of a PT program treats the injury from a different angle and all of the components together contribute to the overall effectiveness of the therapy.
Here are the three injuries we’ll cover:
- Rotator cuff injuries in the shoulder
- Ankle sprains
- ACL injuries in the knee
Without further ado, let’s get started.
How Effective Is Physiotherapy for Rotator Cuff Injuries?
Rotator cuff injuries have a prevalence of 7-30% in the general population. Yet, less than 5% of people with rotator cuff tears seek surgical treatment. Hence physiotherapy is the primary treatment for it.
Physiotherapy is highly effective for rotator cuff injuries. 75% of the patient population (at 2-year follow-up) regain full mobility and strength in their shoulders after PT.
You can expect to see significant improvement in pain and function in approximately 12 weeks, although some people report feeling better after just 6 weeks of rehab.
The rotator cuff has a limited blood supply which slows down its healing. That’s why muscle atrophy (loss of muscle mass) is common in these injuries if you leave them untreated.
The reason PT is so effective here is that the techniques we use increase the blood supply to the injured area and provide it with the necessary nutrients it needs to heal.
Quick overview of the rotator cuff
The rotator cuff is made of tendons and four muscles that surround the shoulder joint from all sides. Its job is to stabilize the joint and allow your arm to rotate and move up to the side.
You can injure it with repetitive overhead activities. Although it’s common in athletes, other people can get it too especially if their job requires too much overhead work.
How Do Physiotherapists Treat Rotator Cuff Injuries?
The conventional management of rotator cuff injuries includes manual therapies, soft tissue massage and exercises.
The usual program is for 2-3 in-clinic seasons during the first few (usually 3-6) weeks and then home exercises every day for 3 months.
Research suggests that it’s best to start rehab exercises early. These include: (Reference)
1. Daily Range of Motion Exercises
You should preferably do ROM exercises actively. But it’s ok to have someone assist you for the first week or so.
To perform, lift your arm in the air by moving it sideways all the way above your head.
Similarly, rotate your arm inwards and outwards while keeping it in the air. Do 10 reps of each exercise and repeat a couple of times a day.
2. Stretching and Flexibility Exercises
To perform the crossover arm stretch, take your arm (of the affected shoulder) and move it across your chest in a way that you touch the back of the opposite shoulder.
To stretch the anterior shoulder, lift your arm along the side of your body up to the level of your head and drive your elbow behind.
Alternate exercise: Stand in a doorway and hold the door frame with your hand. Now step forward so as to stretch your arm and the anterior shoulder.
If you experience pain during or after any exercise, then letting your arm hang freely like a pendulum and moving it back and forth can be soothing.
3. Rotator Cuff Strengthening Exercises
Bilateral external rotation is the most important one in this category.
To perform, lift your arm in the air and rotate it so that your thumb is pointed away from your body. You can progress by holding a heavy object such as a hammer in your hand and doing the same.
Do 10 reps of this exercise, three times a week.
4. Biomechanics Adjustment
This involves working on scapular muscles and upper back posture along with the rotator cuff.
For this, you can perform scapular retraction (squeeze scapula) and scapular shrug exercises, initially without any weight and progress to add free weights in your hands for more resistance.
This exercise program is proven to be effective for decreasing pain and increasing the active range of motion for different age groups (one study had participants of the average age of 25y and the other with 62y). Starting physical therapy early also reduces the need for surgery.
It’s important to note that while you’ll experience a relief in symptoms during this program, the tears in the rotator cuff might still remain. These will heal over a period of weeks or months depending on the thickness of the tear.
Learn about the best exercises to injury-proof your shoulder here 💪
Effectiveness of Physical Therapy for Ankle Sprains
When compared with treatments such as only doing RICE (rest, ice, compression, elevation) after a sprain and no structured exercises, physiotherapy comes out on top as the most effective treatment.
But its effectiveness is established only for certain populations as of yet.
Younger patients tend to recover quickly (reduction in pain in 1 week) with structured exercise programs. While others don’t experience a difference in pain, function, or recovery timeline by doing physical therapy. (Reference)
PT is effective to restore ankle function, improve mobility & balance, decrease pain and increase strength after a sprain much quicker than what you’ll have without physiotherapy.
The timeline to regain full ROM and functional mobility of the injured joint depends on the severity of the sprain.
The ligament heals in its own time (6 – 12 weeks for mild or moderate tears) but physical therapy is effective and safe for managing symptoms, returning you to functional activities and preventing re-injury.
Although we need more research about this condition to design a physiotherapy treatment regimen that’s effective for the majority of people suffering from a sprain, the current program works well for athletes and nonathletes alike.
Components of a Research-Backed Physical Therapy Program for Treating Ankle Sprains
The physical therapy exercise program begins immediately after an ankle sprain. (Reference)
During the acute phase (usually 3 weeks after injury) the focus of physical therapy is on controlling inflammation, re-establishing full ROM, and gaining strength.
For that, we use:
1. Stretching Exercise
Hold the ends of a folded towel in your hands and place your affected foot in the middle of it. Straighten your knee and pull on the towel for 15-30 sec to stretch your ankle. Perform 10-20 reps of this stretch every day.
2. Early ROM Exercises
Sit comfortably with your foot hanging freely. Move your foot up and down, sideways and rotate it as if you were forming circles. Do each for 30 seconds to a minute a couple of times a day.
3. Progressive Balance Exercise
When you can freely move around and use the joint (approx 72h after onset of pain) try to bear your full body weight on your legs. (Reference)
If you can easily do that, then try to stand on one leg for 20–30 seconds and repeat it for 10 repetitions, 3-4 times a day.
Then begins the phase of early functional rehabilitation of the ankle.
This includes strength-training exercises such as:
1. Isometric ROM Strengthening
Place your foot on a stable surface such as your bed or the floor and push downwards.
Your foot should move just the slightest bit during this but the muscles on the back of your lower leg should get tense while you’re attempting to push onto the stable surface.
With your foot on the floor, try to lift the toes and mid-foot off the ground while resisting this with your hand.
Similarly, try to rotate your foot inward and outwards while stopping it with your hand or having someone else resist this motion for you.
Perform 20 reps of each with 10-sec holds.
2. Biometric Taping
Some physiotherapists apply sturdy tape on the outside of the ankle to provide additional support to the ankle joint while you return to activity after a sprain. (Reference)
You’ll start proprioception and balance exercises towards the end of the program. These are effective in addressing muscle strength deficits and recurrence of ankle sprains.
1. Balance Board Exercises
Stand on a wobbly surface and maintain your balance. You can start by standing on a pillow or a cushion and later use balance boards.
2. Progressive Body Weight Strengthening Exercises
Do 10 reps of a partial double-leg squat and then single-leg squats. You can also perform lunges for strengthening the ankle or walk between cones and change direction while walking quickly.
How Effective Is Supervised Physical Therapy for ACL Injuries?
ACL rehab is a hot topic in the physiotherapy community.
Along with sports physiotherapists, many musculoskeletal physios are also heavily involved in it because approximately 69 per 100,000 non-athletes also suffer from ACL injuries.
These are people who’ve been in car accidents and weekend warriors.
Physiotherapy for ACL injuries is effective. 65% of amateur athletes return to play after post-ACLR physiotherapy.
Supervised PT is equally effective as a home-based independent rehab program for this group. (Reference)
But since athletes have to perform on an elite level, supervised physical therapy becomes a necessity for them and is effective for returning them to play.
They need a physical therapy clinic for rehab because they don’t have the necessary equipment at home nor the knowledge to know how to progress safely.
There’s no doubt that rehab is necessary for ACL injuries because reloading the ligament after reconstruction or repair is a sensitive process and requires expertise.
Literature shows that patients who don’t follow a rehab program have poorer thigh muscle strength and circumference in the short and the long term. (Reference)
But the intensity, duration, load, and supervised vs non-supervised rehab are where the effectiveness is unclear.
For instance, research shows that accelerated and non-accelerated programs don’t significantly differ in results at a 2-year follow-up.
Hence physical therapy, or rather a progressive exercise program in a clinical or home setting, is absolutely necessary for rehab of ACL. But the requirement of a physiotherapist during rehab varies widely between populations.
What Does an Evidence-Based ACL Rehab Program Look Like?
ACL rehab programs are always customized for each patient because the injury is highly complex and varies between individuals, and so is the surgery to repair it.
These programs are lengthy and often continue for about a year because 78% of athletes need a year to be ready to return to sport.
Here’s the outline of what’s included in the physiotherapy treatment program for ACL injuries:
It begins with prehabilitation (exercises before surgery) where the goal is to decrease swelling & pain and maintain joint range of motion and muscle strength of the quadriceps.
It includes:
1. ROM Exercises
Flex your knee all the way and then extend it back to full length.
2. Straight Leg Lifts
While laying on a bed, lift your leg in the air and bring it down. Perform 10-15 reps of this every day while holding the leg in the air for 10-30 seconds. It increases quadriceps strength.
3. Static Quads
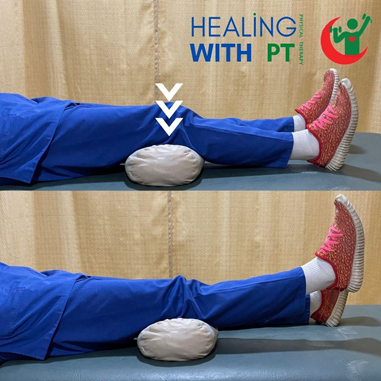
Put a roll underneath your knee while lying down and press down on this roll. Your ankle should lift off the bed. Repeat 10-15 reps with 5-second holds.
4. Leg Extensions
While laying down, put your foot on top of a roll and allow your knee to stay in full extension. Maintain this for 30 minutes or so every day.
5. Walk Normally
Ensure full range of motion of the knee and proper foot positioning.
6. Swimming
Water makes you feel lighter and takes some of the load off your knees while also reducing pain. You should perform quadriceps strengthening and range of motion exercises under water.
The program after surgical repair of the ligament or when the initial pain response decreases includes: (Reference)
1. Cryotherapy and Electrostimulation
These help manage pain immediately after surgery.
It’s wise to note that it doesn’t affect drainage and the current evidence suggests that cryotherapy also doesn’t do much to decrease inflammation.
Learn about the myths about cryotherapy here!
2. Weight-Bearing Begins Immediately After Repair
That’s if you can maintain the normal gait pattern and there’s no additional swelling upon walking for a bit.
3. Isometric Quads Training
This begins in the first postoperative weeks.
4. Closed Kinetic Chain Quadriceps Exercises
Eccentric quad strengthening begins after 3 weeks of an ACL repair.
5. Strengthening Exercises for Lower Limb Muscles
This is done to optimize the body weight distribution on the hips and the knee and to improve your walking pattern.
We won’t explain how each exercise is performed because these are varied amongst patients and it won’t be appropriate to explain them all in one article.
Physiotherapists choose exercises based on a multitude of factors. The strengthening exercises are aimed at:
- Hip flexors
- Hip extensors
- Hip adductors
- Hip abductors
- Hamstring muscles
Strengthening exercises begin with bodyweight exercises but you will need some equipment to perform these later on. This equipment includes resistance bands, leg press, bicycle, steppers, Nordic tracks and treadmills.
6. Balance and Proprioception Exercises
You’ll perform plyometric and sport-specific drills towards the end of the program. These include exercises that involve cutting, changing positions, and jumping.
For non-athletes, balance boards are ideal. You’ll stand on it with both legs and then a single leg.
Your therapist might make it more challenging by throwing a ball toward you and asking you to catch it and throw it back while you’re trying to balance yourself on a wobbly surface.
The Takeaway
Physical therapy is highly effective for most musculoskeletal injuries. Most patients who follow the exercise regimen as prescribed experience a decrease in pain and an increase in mobility. I believe you must have understood that from the details above.
But no two programs or two conditions are the same.
Each condition has its own timeline of recovery and the same condition can have different programs, and different effectiveness, for different populations because one size doesn’t fit all in physiotherapy.
But the bottom line is that PT takes away the pain and optimizes mobility to give your body the time to heal itself.
So if you have a painful injury that’s limiting your function, then visit a physiotherapist and get yourself treated
Disclaimer: This article is for informative purposes only. We provide well-researched and authentic information. Do not consider this personalized health advice. Please contact a licensed healthcare professional for medical issues and health concerns.