Physical therapy has a key role in improving the quality of life of the elderly with exercises and physical activity. And that all begins with proper assessment during the patient intake.
Geriatric physical therapy covers a range of problems such as mobility issues, balance disorders, cognitive issues, cardiovascular diseases, skeletal problems and more.
The evaluation of the older population begins with a subjective assessment to get the patient’s perception of the problem, their demographic information and history. Then the physical therapist performs the objective assessment which we will discuss in this article.
The goal of the assessment is to establish a baseline and measure the treatment outcomes with it. That’s why physical therapists must understand what geriatric objective assessment entails, why it’s different from other assessments and how to perform it efficiently.
Why is Geriatric Objective Assessment Different?
Many of the components of geriatric assessment remain the same as those for the younger populations. But certain areas need additional focus during the assessment of the elderly. These may include cognition, functional independence and physiological health status.
That’s because in most geriatric physical therapy care settings, the goal is to treat the overall individual rather than just presenting complaints. Also, the older patients almost always have coexisting conditions that should be considered while planning out the treatment regimens.
Other benefits of carrying out specialized geriatric objective assessment include:
- Helps physical therapists (PTs) plan an effective holistic treatment approach by clearly identifying the baseline.
- Accounts for comorbidities that may impact the presenting complaint and treatment.
- Improve overall functional outcomes and mobility.
A multidisciplinary team is usually required to properly care for the elderly. Hence, a thorough objective assessment at the time of intake can ensure that your geriatric patients receive the help they need.
The results of the assessment can also help you refer the patient to the appropriate health care professional if need be.
Main Components of Geriatric Objective Assessment in Physical Therapy
Geriatric objective assessment can be time-consuming because there are many systems to check. And the response time of the elderly patients is slow.
That’s why physical therapists should use valid and reliable tools so they can get the most accurate and thorough results without tiring out the patient.
In this section, we’ll cover the main components you should check in the physical therapy geriatric assessment. And also discuss the screening instruments you should use as recommended by the current best evidence.
1. Cognition and Mental Status
13.9% of the elderly above the age of 71 suffer from dementia. And the prevalence of conditions such as Alzheimer’s and depression increases with age, affecting more women than men.
So before you begin your objective assessment, you may want to check the cognition and emotional state of your geriatric patient. That should help you know if the patient will understand your instructions during the assessment. And also give you an accurate picture of the patient’s memory and emotional state.
Before you begin your objective assessment, you may want to check the cognition and emotional state of your geriatric patient. That should help you know if the patient will understand your instructions during the assessment.
The Mini-Cog assessment instrument is one of the best tools to assess the presence of dementia and the level of memory of your patient. It’s brief with a sensitivity of 76% and specificity of 89% and requires minimal training for the administrator of the test.
This test checks memory, language, visual‐motor skills and executive function. The best feature of this test is its adaptability to different languages.[i]
The Mini-Mental State Exam (MMSE) is another reliable and valid instrument to assess the mental status of geriatric patients. It has a sensitivity of 79% and a specificity of 88%. The items checked here include orientation, registration, attention and calculation, recall, language and copying.
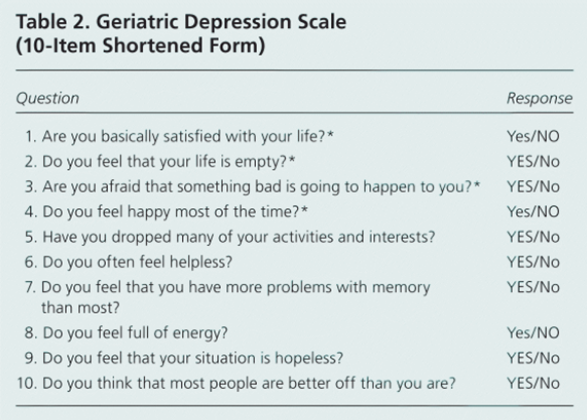
The Geriatric Depression Scale (GDS) is a valid tool to assess the emotional status of elderly patients. It has a sensitivity of 92% and specificity of 91% according to the recent study by Busra Durmaz et al.[ii] The GDS is a 15 item self-report instrument that requires yes and no answers.
2. Physical Exam
Here you should check the height, weight, blood pressure, vision, hearing, nutritional status, range of motion, coordination and sensory status of your patient. Establishing the baseline values can help you gauge the progress effectively.
Most of the areas included in the general physical assessment do not require too many instruments or different tools.
For example, you can use the Snellen eye chart or Jaeger card to check vision, whisper sentences from 6-12 inches away to check the hearing and use the goniometer for checking the range of motion (ROM).
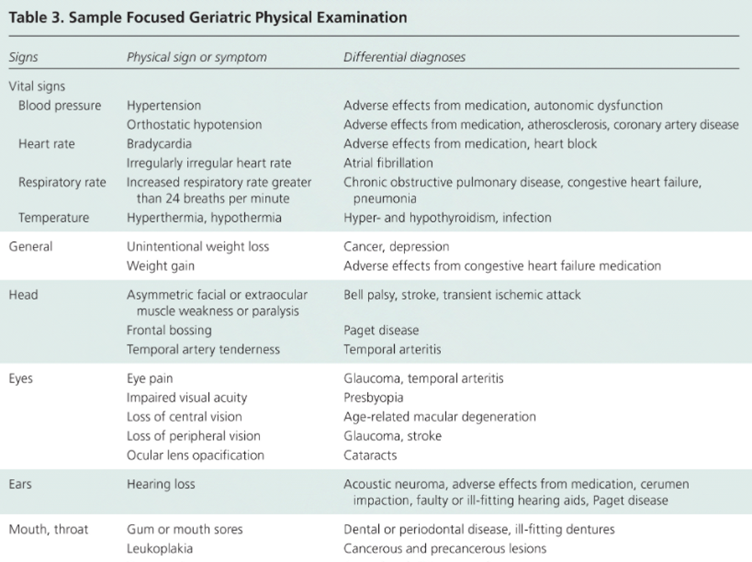
The American Family Physician has an excellent resource that covers the geriatric physical exam in detail along with the relevant instruments. You can read more here.
3. Functional Mobility, Balance and Gait
The aging adults suffer from various mobility issues due to neurological issues, osteoporosis, muscle weakness and joint conditions such as arthritis. That can lead to falls and balance problems and ultimately pose a risk to their safety.
The various assessment tests to check mobility include the timed up and go (TUG) test, short physical performance battery (SPPB), berg balance test and the elderly mobility scale (EMS) to name a few.[iii]
| Validity and Reliability | Intended Purpose | Intended Population | Time of Administration |
| High concurrent validity and good inter-rater reliability[iv] | Assess gait, transfer, balance and mobility in frail elderly | Elderly without major diseases | 15 min |
| Valid with excellent reliability[v] | To assess balance and walking ability | Stroke, Parkinson, Osteoarthritis, vestibular disorders | <15 min |
| Valid and reliable for test-retest [vi] | Balance and gait assessment + identify fallers | Stroke, Parkinson’s, MS, spinal disorders | 10-15 min |
| Valid with high-reliability [vii] | Functional stability during walking + risk of fall | Elderly, stroke, TBI, vestibular disorders | 15 min |
Source: A Systematic Review of Thirty-One Assessment Tests to Evaluate Mobility in Older Adults by Racha Soubra et al.
The elderly mobility scale (EMS) is one of the best instruments physical therapists use to assess the overall mobility of the elderly.
The seven areas covered under the EMS include:
- Lying to sitting
- Sitting to lying
- Sitting to standing
- Standing
- Gait
- Timed walk
- Functional reach
When choosing a test, you must match the appropriateness of the test to your patient and use the test according to the intended purpose for which it was designed.
4. ADLs and IADLs
This category of the functional status exam is best assessed by self-report. For that, you can use the Katz Index of ADL [construct validity of 74% to 88%] or the Lawton-Brody Instrumental ADLs scale.
The Katz Index checks the independence of the patient in bathing, dressing, toileting, transferring, continence and feeding. You have to give one point for complete independence and zero points for dependency.[viii]
The Lawton-Brody IADL scale tests eight areas. These include the ability to use the telephone, shopping independently, food preparation, housekeeping, doing laundry, ability to use transportation, managing medications and finances.
Only a few studies have checked the validity and reliability of this scale. Currently, the inter-rated reliability of the Lawton-Brody IADL scale is 85%.[ix]
Importance of Understanding Geriatric Assessment for Physical Therapists
The number of older adults is increasing faster than ever. Statistics show that there’ll be 1.5 billion older people globally by 2050. That’s 16% of the entire world’s population.
This increasing population means that there will be a larger number of geriatric patients who will need physical therapy services. Hence, PTs should dedicate their time to learning and familiarizing themselves with the special objective assessment requirements of geriatric patients so they can be better health care providers.
PTs also have a big role in preventive medicine.
The healthcare costs for the elderly is nearly triple for the younger populations. Proper systematic assessment of the geriatric can help physical therapists identify vulnerabilities in patients and help them before they need expensive medical treatments.
The healthcare costs for the elderly is nearly triple for the younger populations. Proper systematic assessment of the geriatric can help physical therapists identify vulnerabilities in patients and help them before they need expensive medical treatments.
In Summary
The physical therapy treatment approach for the elderly goes beyond just treating the patient for the presenting complaints.
Rather, geriatric treatment regimens involve various systems. And the preciseness of the treatment protocols depends on the quality of the assessment.
Knowing about the best screening instruments can make sure that you can conduct the assessment quickly and efficiently.
The detailed geriatric objective assessment instruments discussed above should help physical therapists in getting an accurate picture of their patient’s health status which in turn can help them improve functional outcomes by prescribing the appropriate treatments.
[i] https://pubmed.ncbi.nlm.nih.gov/11113982/
[ii] https://pubmed.ncbi.nlm.nih.gov/30688929/
[iii] https://www.hindawi.com/journals/bmri/2019/1354362/
[iv] https://www.sciencedirect.com/science/article/abs/pii/S0031940610606128
[v] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5087865/
[vi] https://journals.lww.com/jnpt/Fulltext/2013/03000/Test_Retest_Reliability_and_Construct_Validity_of.4.aspx
[vii] https://www.archives-pmr.org/article/S0003-9993(07)01447-5/fulltext
[viii] https://www.alz.org/careplanning/downloads/katz-adl.pdf
[ix] https://www.alz.org/careplanning/downloads/lawton-iadl.pdf
