Iliotibial band syndrome (ITBS) is an overuse injury commonly seen in athletes, particularly runners and cyclists. Some people have a much severe form of this condition while other athletes never suffer from it at all. That makes the causes of ITB syndrome somewhat of a mystery.
It’s classified as one of the top three most common knee injuries in runners. It has an incidence rate of 5-14%[i] and it’s most often seen in men than women.
In this article, we’ll answer some of the frequently asked questions about ITBS and give you an overview of what physical therapy (PT) rehab looks like for this condition.
What is the Iliotibial Band (ITB) Syndrome?
The Iliotibial Band is a thick band of fascia on the outside of your leg.

It extends between your pelvis and a little below the knee. It works to extend and abduct the hip. A tightness, inflammation and irritation of the ITB can lead to the Iliotibial Band Syndrome – also sometimes known as the Iliotibial Band Friction Syndrome (ITBFS).
It’s a common condition that often affects athletes who perform repetitive motions involving the knee.
But non-athletes also suffer from ITBS. These include office workers or drivers who sit for extended periods,
The symptoms of ITBS include:
- Sharp pain and tenderness on the outside of the knee.
- Burning sensation just above the knee.
- Worse pain when coming down the stairs or prolonged running.
- Sometimes pain is accompanied by swelling at the knee.
- There may be some audible snapping sound of fascia during flexion-extension.
Physical therapists or other healthcare providers diagnose the ITBS from history and physical examination. They’ll likely move your knee into various positions and do a few manual tests to confirm the diagnosis.
What Causes a Tight ITB?
The exact cause of ITB syndrome is not known.
According to a 2017 scientific paper, the compression of the underlying adipose tissue and the nerves could be a potential cause of ITBS.
Also, Fairclough et al. studied the functional anatomy of the ITB with MRI. They suggested that the Iliotibial Band Syndrome could be the result of fat compression beneath the tract.
This compression of the ITB is most likely at 30° of knee flexion i.e. during the footstrike phase of walking and running. That’s known as the impingement zone. Here, the muscles surrounding the ITB contract eccentrically thus compressing the ITB and the underlying structures.
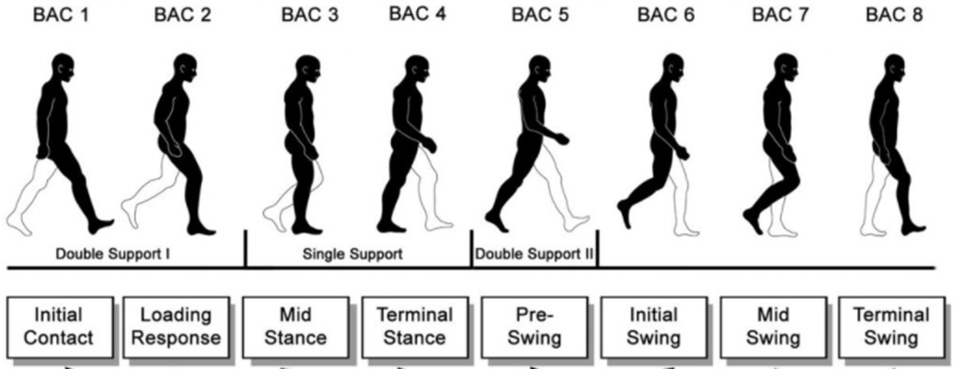
The impingement zone is at the initial contact and loading response phases in this image.
The compression can then lead to friction between the ITB and the bone.
Even if we’re unsure of the exact cause of ITBS, we do know the various risk factors of it based on different research.
Performing repetitive movements with bad form is a primary risk factor for this condition. Some other potential causes include:
- Weak hip abductors.[ii]
- Internal rotation of knee during the stance phase of running.
- Hip or knee joint stiffness.
- Long-distance running.
- Ineffective warm-up and cool down before and after exercise.
- Hiking.
- A sudden increase in activities that involve flexion-extension knee movements.
- Inflammation of the ITB bursa.[iii]
ITBS is a multifactorial injury. So we can’t claim that one specific movement or posture causes this pathology.
Is My Tight ITB Actually a Problem?
Whether your ITBS is an issue for you or not depends largely on your activities.
A slight compression of the ITB that produces pain occasionally only when you perform above usual activities isn’t something you should worry about too much.
Although, you should take it as a warning sign that the condition might become chronic if you don’t take precautionary steps.
Athletes and fitness enthusiasts who perform strenuous exercises every day should take ITBS seriously even when it’s mild. Because it can get worse with exercise and lead to long-term problems if you don’t treat it properly.
Also, if you have significant pain in your thigh or calf then you should immediately visit your doctor or PT.
Remember, ITBS can lead to further complications such as patella femoral syndrome (runner’s knee) if left untreated. So take precautions and follow the rehab guidelines you get from your doctor after the diagnosis.
How Can I Prevent ITB Syndrome?
Proper strengthening and stretching of the ITB and the surrounding structures are some of the best ways to prevent ITBS. Especially if you’re involved with a sport or job that requires more than usual flexion-extension movements at the knee.
Proper strengthening and stretching of the ITB and the surrounding structures are some of the best ways to prevent ITBS.
Some other steps you can take to prevent Iliotibial Band (ITB) Syndrome include:
- Use proper form when exercising such as squatting, running and hiking.
- Always progress at a decent pace and don’t overexert your knee.
- Identify the warning signs and pause long-distance running or cycling to give your ITB ample time to rest or heal.
- Don’t skip stretching, warm-up, and cool down.
- Build strength in your ITB and hip abductors.
What Does ITB Physical Therapy Rehab Entail?
The physical therapy rehab for Iliotibial Band (ITB) Syndrome varies in time and the type of treatment according to the condition of the patient.
There can be different causes and risk factors for ITBS, as we’ve covered above. So physical therapists design the rehab according to the specific issues of the patients.
The treatment of acute ITBS begins with the medical management of the condition. That includes rest, NSAIDs and cryotherapy. Rehabilitation begins once the inflammation has subsided and the pain has decreased enough to tolerate the exercises.[iv]
PT is usually the best line of treatment for most ITBS patients. Overall, here’s what you can expect from a PT rehab program for ITBS:
1. Stretches and activity modifications
Rehab begins with activity modifications.
Physical therapists work with the patient to modify their activities. Not everyone can completely stop their aggravating activities, such as an office worker can’t stop sitting during his work hours. Therefore a modification is the best option in most cases to deload the ITB and allow healing.
Your physical therapist may also recommend active rest. Meaning that you’ll still be active as opposed to bed rest, but you’ll perform activities that don’t overload your ITB. These activities could be swimming or walking instead of running.
Research is a bit conflicted over what the rest period should be with some suggesting complete rest for 3 weeks while others recommending 2 months.
So the duration of active rest depends on your condition and your physical therapist’s assessment of your clinical symptoms.
Stretches were widely used in the initial phases of the rehab. Although, these days their use is less popular as stretches aren’t highly effective. That’s because ITBS’s primary cause is usually a weakness of the surrounding muscles and not a tightness of the ITB.
Anyway, stretches may be helpful to release myofascial restrictions and speed up the rehab in certain cases.[v] The common stretches for ITBS include side-lying leg raises, seated twists and using a foam roller.
2. Massage
Physical therapists use various massage techniques in ITBS rehab.
This help reduce the damage caused by inflammation. It also increases blood flow to the area and prevents muscle adhesions.[vi]
Friction massage also helps maintain the mobility of the soft tissue structures such as the tendons and the ligaments.[vii] That’s especially helpful for chronic ITBS.
Some physical therapists also use the Kinesio tape. It supports the muscles in the correct position while allowing the inflammation to subside.
3. Recommended exercises for ITB syndrome
The final stage of PT rehab for ITBS includes exercises to strengthen the gluteal and other hip muscles.
These include[viii]:
- Clamshell exercise with a resistance band around the knees to strengthen the gluteals.
- Side-lying hip abduction to strengthen the gluteals, anterior hip flexors and tensor fascia latae.[ix]
- Side planks as a more advanced version of the side-lying hip abduction exercise.
- Split squats to work the gluteals, hamstrings and hip stabilizers.
- Plyometrics exercises such as mini squat jumps, lateral jumps and lunges.
You can watch the demonstration of how these exercises are done in this video.
We recommend you don’t start these exercises yourself until you’ve had a physical therapist prescribe them to you.
Tight Iliotibial Band a Problem To Worry About? – The takeaway
The time needed for complete recovery of ITBS varies according to the level of its severity. It also depends on how well the patient follows the rehab program.
You can expect the rehab to take three to six weeks but be prepared for it to take longer.
This article covers an overview of what the ITBS is and what you can expect from the rehabilitation of this condition.
If you’re suffering from pain in the outside of your tight, around the knee or have any symptoms mentioned here, then you should consult a physical therapist or a doctor for an accurate diagnosis.
[i] https://pubmed.ncbi.nlm.nih.gov/22994651/
[ii] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2100245/
[iii] https://pubmed.ncbi.nlm.nih.gov/22134205/
[iv] https://journals.lww.com/jaaos/Fulltext/2011/12000/Iliotibial_Band_Syndrome__Evaluation_and.3.aspx
[v] https://link.springer.com/article/10.2165/00007256-200535050-00006
[vi] https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD003528/abstract
[vii] https://www.jospt.org/doi/pdf/10.2519/jospt.1982.4.1.16