Neurological physiotherapy is a vast field that has a role in rehabilitating patients suffering from acquired or congenital (issues that are present by birth) neurological issues.
Keep reading to learn more about
- What is neurological physiotherapy?
- The conditions that fall under the domain of neurological physiotherapy
- The specific treatment techniques we use for the best results
- How programs are designed while keeping the patients’ end goals as a priority.
What Is Neurological Physiotherapy?
Neurological physiotherapy involves the treatment of movement disorders and physical symptoms that arise due to a brain or nerve problem.
Physiotherapists who specialize in this domain use various techniques aimed at teaching movement patterns to regenerate nerves, balance muscle tone, and improve muscle strength.
The most common physical symptoms of neurological issues are:
- balance problems
- increased stiffness in muscles
- loss of muscle tone
- decreased strength
- lost sensation (feelings in the skin)
- lost muscle power
- pins and needle sensation
- tremors
Although usual physiotherapists can treat patients with neurological conditions, it’s better to go to a neurological physiotherapist.
Research shows that receiving specialized physiotherapy treatment for neurological conditions such as Parkinson’s disease generates better results for the patient in terms of lower complications.
Scope: Medical Conditions Treated Under Neurological Physiotherapy
Here are some neurological disorders treated by neurological physiotherapists.
1. Stroke
The medical term for stroke is Cerebrovascular accident (CVA), also known as ‘brain attack’ in non-scientific terms.
It happens as a result of ruptured blood vessels in the brain. That causes some parts of the brain to be deprived of oxygen and nutrients while other parts suffer a hemorrhage (blood clot formation)
The symptoms of stroke that physical therapists treat include:
- Balance and coordination problems.
- Weakness, muscle power loss on one side of the body, and later increased stiffness.
- Skin sensation loss in one side of the body along with pain, burning, and tingling sensation.
- Partial loss of facial expressions and related issues with speech and swallowing problems.
Patients who suffer from stroke often start neglecting the affected side of the body. We work with them to break that habit and use specialized neurological techniques (discussed in the next section) to restart movements in the affected regions.
Read about the physical therapy treatment of Stroke patients in detail by clicking here.
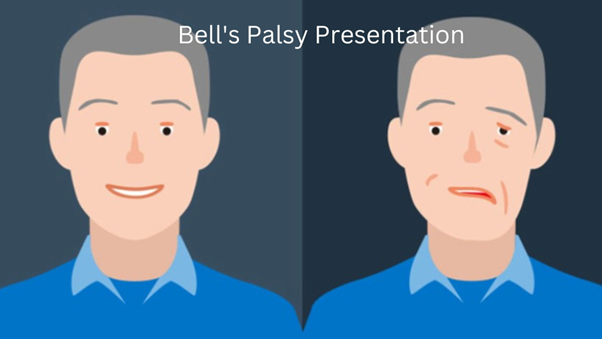
2. Bell’s Palsy
A temporary loss of sensation and muscle power in one side of the face is called Bell’s Palsy. It can be caused by multiple factors such as an ear infection, or damage to the facial nerve (it supplies the muscles of the face).
Here are the physical symptoms associated with Bell’s palsy that neurological physiotherapy treats:
- Muscle weakness or paralysis on one side of the face
- Difficulty closing mouth to drink fluids that causes drooling and inability to smile symmetrically
- Unable to expand or contract nostrils on the affected side
- Difficulty frowning and closing or opening the eyelid on one side
- Loss of facial expressions on the affected side
Most patients with Bell’s Palsy have an excellent prognosis. Some studies found improvement within 3-4 weeks post-onset and complete recovery within a couple of months.
3. Cerebral Palsy (CP)
This is a condition in which patients suffer from mild to severe physical and cognitive deficits. It can be due to a lack of oxygen to the brain at birth, in-uterine developmental issues, exposure to toxins, etc.
The physical symptoms associated with Cerebral Palsy that are treated by a neurological physical therapist include:
- Muscles are either too stiff or floppy
- Muscle weakness especially if those required to maintain posture
- Jerky movements (sudden stops, movement suddenly becomes too fast or too slow, movements aren’t controlled as are in a physically healthy person)
- Delayed milestones
- Tiptoe walking and lack of fine motor skills
Since cerebral palsy is a lifelong condition, our goal is to improve the quality of life of both the patient and the caregiver.
For that, we work in a multidisciplinary team with occupational therapists, behavioral therapists, and physicians. Physical therapy continues for life for such patients and the techniques change with changes in symptoms.
4. Cauda Equina Syndrome
The spinal cord ends in the low back region. A collection of nerves continues to supply the lower limb and that’s known as Cauda Equina.
A break in the continuity of the backbone during the development of the fetus causes these nerves’ (spinal cord) to form a balloon outside of the spine.
That results in varying degrees of weakness and loss of sensation in the areas supplied by cauda equina. Damage to these nerves can also happen in adults as a result of injury, surgery, spinal anesthesia, etc.
The physical symptoms of cauda equina are treated by physical therapy. These include:
- Weakness or paralysis of muscles in the lower limb
- Coordination and balance issues while sitting, standing, and walking
- Tingling sensation in the lower limb
The level of recovery in patients with saddle anesthesia varies according to the intensity of the problem. We design exercise programs based on the specific issues each of our patients has.
5. Sciatic Nerve Irritation
One of the nerves supplying the lower limb is the sciatic nerve. It has multiple nerve roots in the low back and buttock region.
It can get irritated at the nerve root or anywhere along its path. As a result, you might suffer from physical symptoms on the affected side such as:
- Tingling, burning, or pins and needles sensation at rest and on movement
- Muscle pain along the path of the nerve which means in the low back, along the buttock, the back of the thigh, and behind the knee.
- Numbness in the lower limbs
Sciatica is a common condition with a lifetime incidence of between 10% to 40%.
It usually resolves with physical therapy and proper precautions. The symptoms listed above fall under the umbrella of neurological physical therapy.
6. Radial Nerve Palsy
The radial nerve is one of the main nerves of the upper limb. It passes from the axilla (armpit), travels down the arm on the posterior side (the side with triceps and less muscle belly in your forearm), and supplies the hand laterally (on the side of the thumb).
The radial nerve is responsible for extending your elbow, wrist, and fingers. Damage to this nerve is called Radial Nerve Palsy and its symptoms include:
- Muscle weakness in wrist and fingers
- Numbness around the triceps, side of the arm, thumb, and first two fingers
- Unable to pinch
- Wrist drop (you can’t move your wrist into an extension so it’s pulled towards gravity)
Neurological physical therapists are trained in helping patients with these symptoms.
The physical therapy treatment for radial nerve palsy is effective but only if you start therapy early on. (Reference) Otherwise, your hand can develop permanent deformities or weakness.
7. Peroneal Nerve Injury or Compression
The peroneal nerve is a branch of the sciatic nerve. It supplies the muscles and the skin in some areas of the leg and the top of the foot.
It can get irritated or compressed due to a knee problem, fracture of the leg, or something causing external pressure on the leg.
Peroneal nerve compression can present as:
- Foot drop because the muscles that lift the ankle upwards (dorsiflex) can’t receive signals to do so
- Numbness and pins and needle sensation in the areas supplied by the nerve
- Weakness in muscles innervated by the peroneal nerve
The symptoms of a peroneal nerve compression vary based on the degree of compression. Most of them are treated by neurological physiotherapy.
8. Ataxia
This is a problem with muscle control due to damage to the brain. It can happen as a complication of stroke, Parkinson’s, alcohol intake, medications, hereditary factors, etc.
The symptoms of Ataxia that neurological physical therapists can treat include:
- Loss of hand coordination
- Loss of fine motor skills necessary for activities of daily living.
- Balance issues in sitting, standing, and walking
- Unsteadiness while moving
Ataxia as a secondary complication of other neurological issues can be a lifelong condition and you’ll need continuous physical therapy to manage the physical symptoms.
9. Migraines and Headaches
Migraines can be due to several reasons such as a lack of sleep, fatigue, an overstimulated environment, overactivity of brain cells, dehydration, etc.
Neurological physical therapists treat migraines and headaches that have a physical cause. The symptoms include:
- Debilitating headache
- Unsteadiness in walking
- Vertigo and dizziness
Our neurological physical therapy treatment for migraines focuses on the root causes of the pain.
It includes manual therapy techniques to relieve nerves that are trapped between tight muscles or bones of the neck.
Neck muscle tightness causing headaches? Read this post to reduce neck tightness at home.
Treatment Techniques & Exercises in Neurological Physiotherapy
Neurological physiotherapy treats the physical symptoms of neurological disorders. But the end goal is usually to fix the damaged nervous structures.
The duration and intensity of physical therapy that a patient needs depends on their symptoms.
Every patient suffering from the same disease doesn’t require physical rehab.
For instance, approximately 85% of stroke patients require physical therapy to regain their movements. But the rest 15% often don’t because their physical symptoms are mild and resolve on their own.
Here are some techniques we use in neurological physical therapy:
1. Stretching and Strengthening
Damage to the nerve or brain means that the muscles won’t receive the signals required for movement. This causes excessive tightness or floppiness in the muscles.
We use stretching and strengthening exercises to treat that. If there’s no movement at all, then we use passive limb exercises where we move the joint through its full range of motion to ensure that muscle contractures (extreme stiffness) don’t develop.
If there’s some level of active movement, no matter how mild, then we use active or active assisted stretching and strengthening exercises.
These exercises help build strength in muscles while the brain and nerves heal as well. Muscles tend to lose their flexibility if they stay immobile for a long time. Stretching exercises help counter that.
For example, we use facial mobility exercises for patients suffering from Bell’s Palsy or facial paralysis. These include making vowel sounds, tightly closing the eyes shut, flaring up the nostrils, smiling against a resistance such as a therapist’s hand on the patient’s cheek, etc.
Similarly, we get our patients with cerebral palsy to lie on their tummies and lift their heads against gravity to build neck-holding strength.
2. Gait and Balance
We use multiple devices in neurological physical therapy clinics to improve balance and coordination. The primary technique is to relearn patterns by breaking them down into steps.
Balance and coordination training play a major role in the rehab of patients with ataxia and stroke.
Some ways we use in neurological physical therapy to train balance and gait (walking) include:
- Balance boards (wobbly boards)
- Treadmill walks with support
- Sit-to-stand
- Standing with a small base of support
- Standing heel-to-toe
- Walking along a line
- Stepping in boxes
Some activities we use for training coordination include:
- Fixing shaped pegs in holes
- Passing a string through a circle
- Moving objects from one box to the other
- Training activities of daily living such as buttoning a shirt and combing hair are activities we use for training coordination.
We also train you to use canes and crutches especially if the chances for full recovery are minimal.
3. Spasticity Management
Sometimes, a damaged nervous system causes excessively increased muscle tone, locking your muscles in place. It’s called spasticity. It’s common in patients with stroke and children with cerebral palsy.
We treat that using various muscle stretching techniques mixed with regular activities. Increasing muscle length can positively contribute to reducing spasticity.
Orthotics and splinting help to position the body in certain postures, often lengthened ones, while the medications do their work to reduce spasticity.
Some additional techniques we use to manage spasticity in neurological physiotherapy include:
- Electrical stimulation of the muscles on the opposite side
- Resistance training,
- Aquatic therapy
- Constraint-induced muscle training (restricting the good limb to promote activity in the affected limb), and biofeedback.
4. Patterns and Repetitions
Neuroplasticity is a phenomenon that states that the neural network in the brain can rewire itself with enough time and training.
Keeping that in mind, we use patterns and repetitions to rehabilitate the damaged nerves and neural structures. (Reference)
For example, for rehabilitation after a stroke, we repetitively perform the same action such as picking up a glass from a table. This helps the body create a new neural pathway to perform this basic activity.
Similarly, exercises for a child with cerebral palsy involve repetitively lifting the head off the floor and practicing sitting down to achieve those milestones.
5. Clinical Electrotherapy
Transcutaneous Electrical Nerve Stimulation (TENS) and Electric Muscle Stimulation (EMS) are widely used in neurological physical therapy rehab.
These help regenerate the nerves and activate muscles while the nerves are impaired, which contributes to muscle education. (Reference)
We use TENS for treating bell’s palsy and use EMS for post-stroke rehab to activate damaged brain areas. The intensity of the current, frequency, and other parameters are adjusted according to the specific condition we want to treat.
6. Simulators and 3D video games
In neurological physical therapy, even trying to move your body is enough to stimulate the nerve and promote regeneration. Since neuro rehab takes a long time, repeatedly trying to move certain body parts without any actual movement can be discouraging for patients.
That’s why we use simulators to make rehab fun and engaging. (Reference)
We strap the affected region of the body to a controller and connect electrodes to the skin before turning the simulator on.
An example of a simulator is a stationary bicycle with a big screen attached to it that shows an open road and an avatar of a person cycling. Every time you pedal or try to pedal, the electrodes from your skin recognize nerve activity and you can see the avatar moving.
Or a VR set that shows a hand holding a glass every time you try to close your fingers to hold an imaginary glass.
How Are Exercises Prescribed in a Neurological Physiotherapy Rehab Program?
The first rule of prescribing exercise in physical therapy is to always tailor them to the person and their condition.
Neurological rehabilitation begins with a thorough assessment which includes evaluating the patient’s natural functions, activities, activity participation, spasticity, joint range of movement, sensation, pain, etc.
Then we design the program based on several factors, the most important of which are their end goals, home environment, and the kind of help they have from skilled nurses, physiotherapists, or caregivers.
We monitor the changes in your baseline levels over time and adjust exercises in different stages of the disease.
This is one of the most important steps in planning rehab programs to provide the highest quality of care. Systematic and frequent changes in the exercise regimen ensure efficient and timely rehab. (Reference)
We also focus on including exercises to prevent secondary complications due to neurological impairments. And keep increasing the intensity of exercises to progressively return you to full function.
The Takeaway
Neurological physical therapy is a vast field that has some similarities to other domains in terms of exercise prescription. You should always visit a licensed expert for medical issues, particularly related to neurological rehabilitation because it can impact your level of recovery and timeline.
Feel free to contact us if you’re suffering from a neurological issue and want a physical therapist to treat it or to get a second opinion about your rehab program.
Disclaimer: This article is for informative purposes only. We provide well-researched and authentic information. Do not consider this personalized health advice. Please contact a licensed healthcare professional for medical issues and health concerns.